Blog
Mesenchymal Stem Cells in Kidney Disease
By Dr Karen Lui – SEP 2023

Our kidneys are an extremely important organ for our body’s detoxification. Every day, about 140 litres of blood get filtered through our kidneys, thereby removing waste products and keeping us alive. Needless to say, our kidneys functioning well is crucial for us to maintain our health.
However, there can be diseases and conditions that may cause damage and affect the functioning of our kidneys. In some cases, if the insult is removed quickly, the injury may be reversible. However, for cases of chronic kidney failure, it is usually a gradual loss in kidney function, resulting from chronic illnesses such as diabetes and hypertension, or autoimmune diseases, such as SLE. In most cases, a person does not even realise they have kidney disease until the condition is advanced.

Source: Medicover Hospitals
The most dreaded end complication of chronic kidney disease is end stage renal failure, which would require dialysis.
In recent years, researchers have realised the potential of stem cells as a modality of treatment for chronic kidney disease, potentially helping patients to improve their quality of life, preserve kidney function, and delay or even prevent the need for dialysis. Stem cells are able to self-renew, and develop into functional kidney cells.
According to a study done in 2020, stem cells are able to repair renal injury by differentiating, repairing damaged cells and by secreting bioactive paracrine factors and releasing microvesicles with regenerative properties.
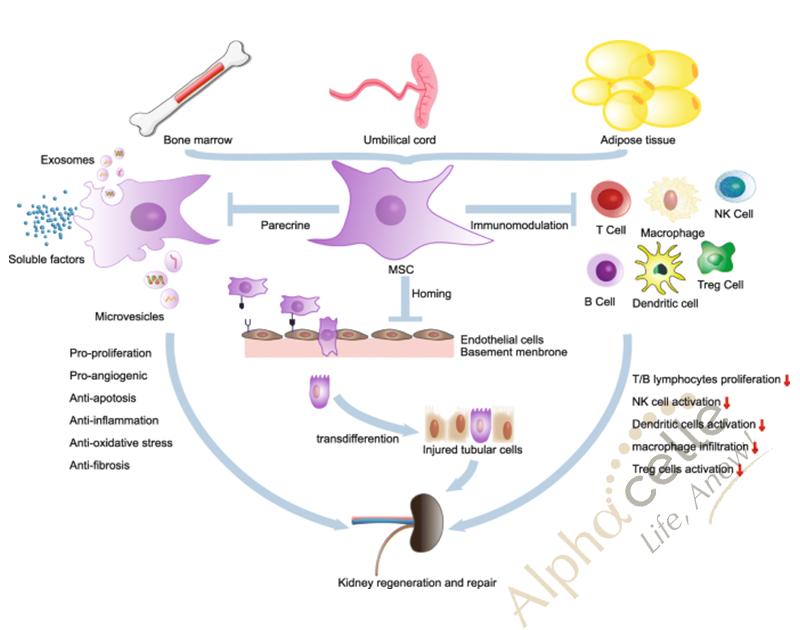
In addition, the study found that treatment with intravenous MSCs managed to efficiently induce improvement of the kidney both morphologically and functionally.
In another study, it was found that umbilical cord MSCs are ideal as they have low immunogenicity, and are able to protect the kidney cells, along with increase the glomerular filtration rate, thereby improving kidney function. They are able to prevent disease progression.

Multiple clinical trials done have demonstrated the safety and tolerability of stem cells, and in particular, MSC based therapies in patients with renal diseases.
In conclusion, stem cell therapy is a safe and promising way to treat chronic kidney disease, by their regenerative and immunomodulatory properties. With stem cell therapy, patients can maintain their health, and look forward to a much better quality of life.
Sources:
Stem cell therapy and Osteoarthritis
By Dr Karen Lui – SEP 2023

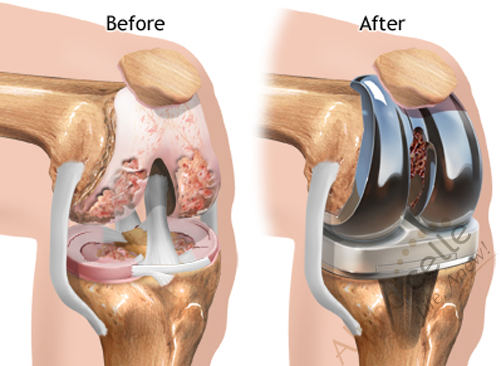
Osteoarthritis is a debilitating, chronic condition whereby there is inflammation, pain, and disability of the joints. It can occur in any joint, but more commonly in the knees, hips, and spine. There are many factors that predispose to osteoarthritis, including older age, female, obesity, genetics, injuries, and repeated stress on the joint. However, age, gender, and genetics are all non-modifiable risk factors for a person to get osteoarthritis.

Source: https://www.bumrungrad.com/en/health-blog/january-2015/knee-osteoarthritis
The most common treatment modality is physiotherapy, exercises, and if the condition gets too severe, a person may have to undergo joint replacement surgery. However, this can be painful, costly, and may not completely resolve the issue, as 20% of people report feeling unsatisfied with the outcome of their joint replacement surgery.
Source: https://medlineplus.gov/ency/article/002974.htm
In recent years, there has been much research done on stem cell therapy for the treatment of osteoarthritis, in particular, mesenchymal stem cells, due to their differentiation capabilities, and their ability to reduce inflammation.

Source: https://www.frontiersin.org/articles/10.3389/fbioe.2019.00009/full
According to a review done in 2022, researchers followed up a group of 329 participants who did intra-articular stem cell therapy for knee osteoarthritis, and followed up on these patients for 24 months. They found that the stem cell therapy was well tolerated, safe, and patients showed significant pain and functional improvement, even in those with severe OA. (1)

Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7868850/bin/ajtr0013-0448-f1.jpg
In a separate review done in 2021, researchers determined that MSCs are good therapeutic agents as they are able to stimulate cartilage production, vascularization (form new blood vessels), reduce inflammation. In addition, there has been no serious adverse events, but instead, an improvement in pain scores and improvement in the OA after receiving umbilical cord mesenchymal stem cell therapy. There was no recurrence of knee pain during follow up of these patients. (2)
As untreated OA will not heal on its own, and there are limited treatment modalities to address the lack of vascularization of cartilage tissue, stem cell therapy remains a promising option for regeneration of joint tissue, as they are well tolerated by our immune system and do not cause any adverse effects. (4)
Sources:
Stem cell therapy for sexual function
By Dr Karen Lui – SEP 2023

Erectile dysfunction is a common condition affecting more than 50% of men between 40 and 70 years old. It can be caused by stress, emotional reasons, or limited blood flow to the penis. It can also be due to chronic illnesses, such as atherosclerosis, diabetes, hypertension or heart disease.

Source: https://novavidath.com/services/stem-cell-therapy-ed/?lang=en
As it is such a common problem, stem cell therapy has been extensively researched for the treatment and use in cases of erectile dysfunction. As such, it has been shown that stem cells are an attractive choice to treat erectile dysfunction due to the self-renewal property and ability to differentiate into a variety of cell types. Mesenchymal stem cells can promote tissue regeneration by releasing growth factors, chemokines, and cytokines.

Treatment of erectile dysfunction patients with mesenchymal stem cells have been found to cause a significant improvement in erectile function and morning erection. These were measured as hemodynamic parameters (mean penile arterial flow) and via sexual function questionnaires. There are also no side effects reported when the stem cells are injected intravenously.
There was also been a review done whereby it was shown that stem cells can help in erectile dysfunction by improving angiogenesis (increasing the number of new blood vessels).
Apart from this, stem cell therapy may also help in erectile dysfunction by improving on the underlying causes to begin with. As they are able to help in diabetes, hypertension, and improve vessel elasticity, stem cell therapy can address the underlying causes of the erectile dysfunction, and prevent worsening of the condition. In fact, by treating these chronic conditions early, we can ensure that the risk of getting erectile dysfunction decreases.
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9963846/#:~:text=In%20a%20general%20manner%2C%20interventional,IIEF%2D15%20or%20EHS
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7825548/
- https://www.news-medical.net/health/Regenerative-Therapy-for-Erectile-Dysfunction.aspx
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4708247/
Mesenchymal Stem Cells for Stroke Recovery
By Dr Karen Lui – May 2023

WHAT IS STROKE?
A stroke, also called a cerebrovascular accident, occurs when the flow to the brain is blocked. A stroke is a serious, life-threatening medical condition and a medical emergency, as it can lead to disability such as impaired speech, weakness or paralysis of the limbs, difficulty to communicate, and worst of all, may lead to death. According to the latest WHO data published in 2020, stroke deaths in Malaysia reached 12.85% of total deaths.

How stroke affect the brain?
After a stroke, millions of brain neurons die while some tissue around the area may be inflamed and non-functioning. Research has found that stem cell therapy may be able to help, by targeting the inflamed and damaged areas. Stem cells are able to promote neurogenesis and replace the neurons lost due to stroke, due to their differentiation capabilities. Stem cells are also able to protect surviving neurons and improve neurological recovery.
Mesenchymal stem cells promote stroke recovery
Mesenchymal stem cells (MSCs) have been shown to enhance neurogenesis, and in particular when they are administered intravenously, as it is the safest and most feasible route for administering stem cells. In addition, MSCs have demonstrated immune-modulatory properties, which is important because our body’s immune system exacerbates the initial damage caused by stroke, thus, the MSCs can prevent further damage.

Furthermore, mesenchymal stem cells play a critical role in functional recovery due to their ability to induce angiogenesis, which is the growth of new vessels in the damaged areas of the brain after a stroke. Stem cells also release large number of growth factors, molecules, and proteins that enhance our body’s natural mechanisms of recovery.

Stem cell therapy has been proven to be a safe and effective modality of treatment to reduce the complications of a stroke. This is due to their immune-privilege, and they do not cause any acute or chronic reactions. Studies have also shown that patients with post stroke who received stem cell therapy had a greater overall survival rate when compared to a control group of patients.
In conclusion, stem cells are a feasible and safe method of treatment in stroke patients, leading to better functional outcomes and a reduction in complications.
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6815222/
- https://www.elsevier.es/en-revista-medicina-universitaria-304-articulo-current-state-perspectives-stem-cell-S1665579616300710
- https://www.flintrehab.com/stem-cell-therapy-for-stroke/
- https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02876-2
- https://www.frontiersin.org/articles/10.3389/fnins.2020.00473/full
Cardiovascular Disease and Mesenchymal Stem Cells
By Dr Choo – May 2023

What is Cardiovascular disease?
Cardiovascular disease (CVD) refers to a group of disorders that affect the heart and blood vessels, usually involving build up of fatty deposits inside arteries and an increased risk of blood clots. Examples of CVD include myocardial infarction (MI), heart failure.
MSCs are a type of multipotent stem cell that can be isolated from various tissues, including umbilical cord tissue, adipose tissue, and bone marrow. They have the capacity to differentiate into multiple cell types, including heart muscle, blood vessels, bone, cartilage, and fat cells, and possess immunomodulatory properties. Additionally, MSCs secrete various growth factors and cytokines that promote tissue repair and regeneration (paracrine activity). On top of that, MSCs have anti-inflammatory properties, which can help prevent the progression of CVD.

In addition to their direct effects on tissue repair and regeneration, MSCs have been shown to have indirect effects on the immune system. For example, MSCs can modulate the activity of immune cells, such as T cells and dendritic cells, which play important roles in the pathogenesis of CVD. By modulating the immune response, MSCs can reduce inflammation and promote tissue repair.
In short, MSCs have emerged as a promising therapy for CVD due to their ability to promote tissue repair and regeneration, modulate the immune response, and reduce inflammation.
Myocardial Infarction and Heart Failure
Myocardial Infarction (MI) refers to the death of heart cells following an event (frequently due to an occluded heart blood vessel) leading to loss of blood supply/oxygen (ischemia) to the heart cells. Although the patient might survive the episode of MI (thanks to our advancing medical technology and medications), the fact remains that MI is an evolving disease. After the ischemic event, anaerobic conditions rapidly induce massive cell death, not only involving cardiomyocytes (CMs), but also vascular cells.

Although a compensatory activity is exerted during the first stages of the disease and may even manage to partially restore functionality, the resulting scar is never repopulated, leading the patient towards the setting of heart failure. Thus, though not conventionally regarded as such, cardiac disease is a degenerative disease in which lack of sufficient contractile and vascular cells leads to a decompensated neurohormonal microenvironment, which further impairs both organ function and cell survival.
What Do MSCs Have to Offer to Cardiac Regeneration?
To achieve the goal of cardiac tissue regeneration, there are three objectives that must be addressed, namely:
(i) the production of a replacement myocardial mass,
(ii) the formation of a functional vascular network to sustain it, and
(iii) the returning of the impaired ventricle to its proper geometry.

Figure 1
Main MSC actions on injured myocardium. MSCs are able to secrete therapeutic substances (paracrine) and differentiate into new blood vessels which encourage healing of damaged tissue and avoiding transition to scar tissue.
MSCs from allogeneic (not from self) origin have been tested and the safety of the procedure was proven, showing fewer episodes of ventricular tachycardia (life-threatening heart electrical activity) and even a better lung function in the cell-treated group. Importantly, a significant increase was detected in the ejection fraction (EF) (indicator of heart function) of the treated patients with reversal of scarring after 6 months of treatment. MSC were also shown to reduce the rate of death by 36 %, reduce incidence of readmission to hospital by 34 %, improved daily life symptoms of heart failure, endurance, and increase heart function in patients with systolic heart failure when compared to placebo.
MSC is a promising form of therapy for those with cardiovascular disease due to its safe nature and potential for regeneration, and prevention of adverse remodelling of the heart. Having said that, cell dose and timing for treatment are critical. Increased benefit is seen for dosing of 100 x 106 (100 million) cells compared to lower doses, and also if the cells are infused during the first week after the infarct. Comparative studies have also shown that cells from young healthy donors (eg Umbilical cord) may yield better effects than stem cells derived from self as it may be defective.
References:
Mazo, M., Araña, M., Pelacho, B., & Prosper, F. (2012). Mesenchymal Stem Cells and Cardiovascular Disease: A Bench to Bedside Roadmap. Stem Cells International, 2012, 175979. https://doi.org/10.1155/2012/175979
Fan, M., Huang, Y., Chen, Z., Xia, Y., Chen, A., Lu, D., Wu, Y., Zhang, N., Qian, J., & Ge, J. (2019). Efficacy of mesenchymal stem cell therapy in systolic heart failure: A systematic review and meta-analysis. Stem Cell Research and Therapy, 10(1). https://doi.org/10.1186/s13287-019-1258-1
Mesenchymal Stem Cells in the Treatment of Diabetes
By Dr Karen Lui – March 2023

Diabetes mellitus is one of the most serious non communicable diseases, affecting approximately 463 million adults worldwide in 2019, and expected to rise to 578 million by 2030.
In Malaysia alone, the prevalence of diabetes mellitus ranges from 7.3%-23.8%. This is a very serious statistic, as it puts these individuals at a high risk of developing a multitude of complications, such as heart disease, stroke, increased blood pressure, narrowing of vessels (atherosclerosis) and nerve damage (neuropathy). In addition, diabetes can affect every organ in the body.
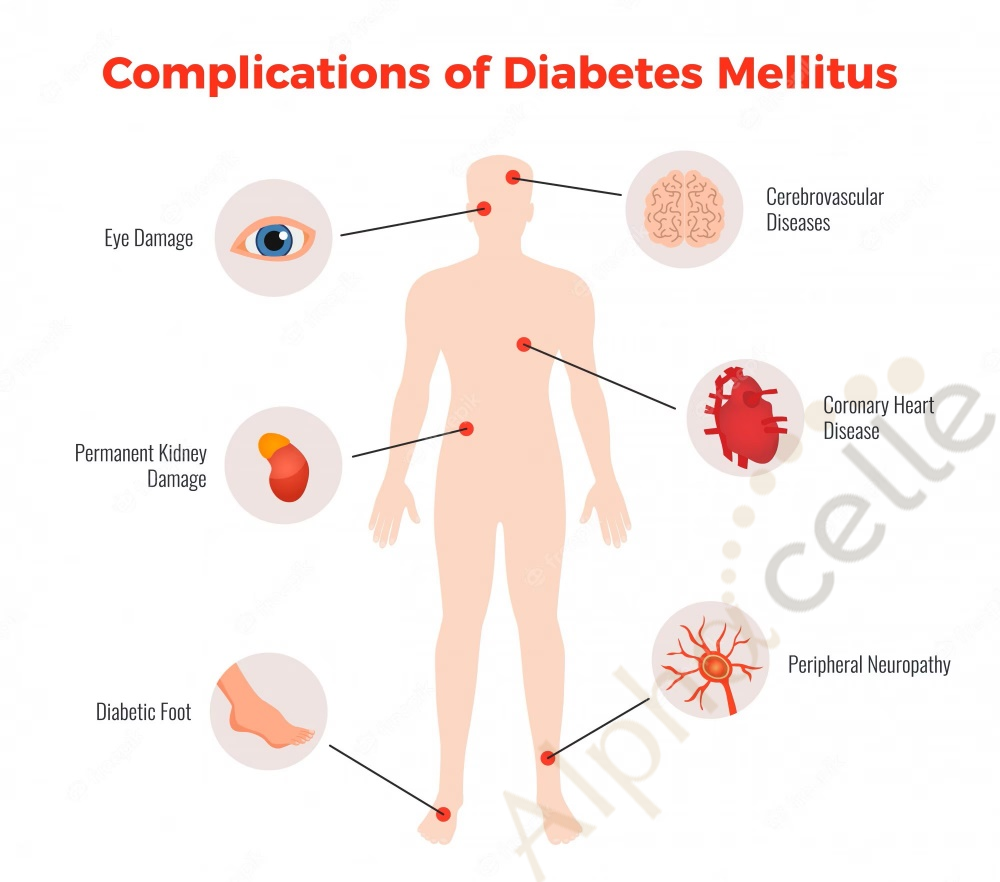
How diabetes is treated ?
To date, there is currently no cure for diabetes. While some opt for the standard treatment of anti-diabetic medication, the body will gradually develop resistance and they will eventually have to start using insulin injections. However, in recent years, researchers have recognised that there is an exciting and great potential in using mesenchymal stem cells for the treatment of diabetes.

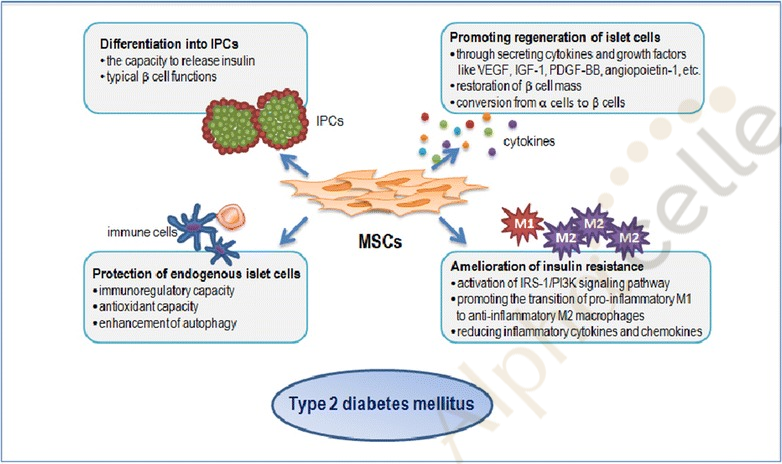
mesenchymal stem cells in the treatment of diabetes
Mesenchymal stem cells (MSCs) are multipotent stem cells that have the ability to self renew and exhibit multilineage differentiation. In the context of diabetes, MSCs are able to regenerate pancreatic islet beta cells, protect endogenous pancreatic islet beta cells from apoptosis, and ameliorate insulin resistance of peripheral tissues. In this way, they are an extremely promising treatment in diabetes.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5433043/
what is the therapeutic potential of mesenchymal stem cells for diabetes?
Over 15 trials currently registered on clinicaltrials.gov have demonstrated that MSCs have shown tolerable safety and efficacy in treating diabetes.
Usage of MSCs in diabetes have shown that patients showed improved glycemic control, improved HBA1C values, and reduced insulin requirements. Treatment with MSCs during the early phase of disease have been shown to restore beta cell function, ameliorate the destruction of pancreatic cells, regenerate the damaged cells, and MSCs can reduce insulin resistance in the body.

Source: https://www.frontiersin.org/articles/10.3389/fendo.2021.646233/full
Insulin resistance leads to chronic, low grade inflammation in the body, and can also lead to obesity and other complications of diabetes. Hence, addressing and treating the insulin resistance is an extremely important aspect of treatment of diabetes. MSCs alleviate insulin resistance by regulating the expression of genes in peripheral insulin target tissues.
In conclusion, results available from the studies are encouraging, and MSCs are a promising mode of treatment for patients with diabetes to achieve better control of the illness, thus improving quality of life.
Sources:
Dementia and Alzheimer’s Disease
By Dr Choo – March 2023

What is Dementia?
Dementia is a broad umbrella term and a syndrome which consists of a constellation of symptoms due to underlying brain degenerative process, but it is not a diagnosis in itself. The diagnosis of dementia often means the patient’s symptoms have very much affected their activity of daily living such as being unable to manage finances, attend appointments or even prepare a meal.
Prevalance of Dementia in Malaysia
In the year of 2020, about 204,000 people in Malaysia was diagnosed with dementia and needs 24-hour care. This number is projected to go up to 637,500 in 2050. About 14.3 % of the population above 60 years old has dementia. According to statistics from the US, this number goes up to 32 % in the population aged 85 years and above. In China, in the year 2019, Alzheimer’s disease and dementia was ranked 5th in the top causes of death.
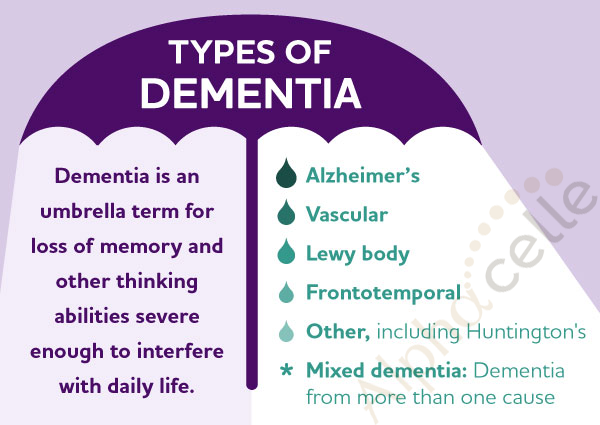
What are the Common Types of Dementia?
Alzheimer’s disease (AD) is a neurodegenerative disease responsible for 60-70% of the 50 million cases of dementia worldwide. It is characterized by neuronal cell death, shrinkage of brain tissue, and progressive cognitive, motor, and behavioral impairment, which often leads to death.
Approximately 60-70 % of all dementias are due to Alzheimer’s disease. The second most common is vascular dementia, which sometimes also occurs in tandem with Alzheimer’s disease, hence the term mixed dementia. Other types of dementia include: Lewy body dementia, frontotemporal lobe degeneration, and dementia due to other causes (nutritional/electrolyte, thyroid, tumour, poison/medication induced). AD is a neurodegenerative disease characterized by the accumulation of extracellular amyloid plaques primarily composed of amyloid-beta (Aβ) peptides and intracellular neurofibrillary tangles (NFTs) of hyperphosphorylated tau protein.
Source: Alzheimer’s Association
What are the Symptoms of Dementia?
Typical symptoms include:
· Memory lapses
· Forgetfulness
· Visual-spatial dysfunction
· Aphasia
· Loss of concentration
· Vision dysfunction
Is Dementia Reversible?
As of today, disease-modifying treatments capable of altering the underlying disease pathology of AD are not available.
What You Can Do to Prevent Dementia?
Prevention strategies include having adequate and restful sleep (deep sleep), cultivating brain stimulating hobbies, having regular meaningful social interactions, having a balanced diet, exercising regularly, avoiding overconsumption of alcohol, optimal management of non-communicable disease and preventing head injuries.
Sleep Well – Reduce Your Risk of Dementia and Death
A research at Harvard Medical School found that individuals that slept 5 hours or less were twice as likely to get dementia and die. A multinational study (France, UK, Netherlands, Finland) found that sleeping 6 hours or less increased risk for dementia by 30 %. One study from Toronto and Chicago even found that in those at higher genetic risk for Alzheimer’s, just by having enough sleep was enough to reduce the likelihood of getting the disease, and was correlated with reduced density of neurofibrillary tangles.
Stem Cells Therapy & Electric Potential Therapy for Dementia
Currently, clinical studies are investigating the role of Mesenchymal Stem Cells (MSCs), exosomes and electric field therapy on prevention of Alzheimer’s Disease, dementia and other neurodegenerative disorders with promising results.
Mesenchymal Stem Cells Slow Dementia Progression
Mesenchymal stem cells (MSCs) are a group of multipotent stem cells capable of differentiating into nonmesenchymal lineages. MSCs are considered a very promising approach to stimulate neuroregeneration due to their immunomodulatory properties and high biosafety but also because of their ability to synthetize neurotrophic and proangiogenic factors. In AD, stem cell therapies have attempted to replace neurons that have been impaired or lost. MSC-based therapies have shown potential to restore damaged neural tissue as well as slow disease progression. In AD models, the reduction of Aβ plaques, β-secretase, and tau hyperphosphorylation as well as the reversal of microglial inflammation, and the stimulation of anti-inflammatory cytokines are among the mechanisms postulated to have a therapeutic effect in MSC therapy.
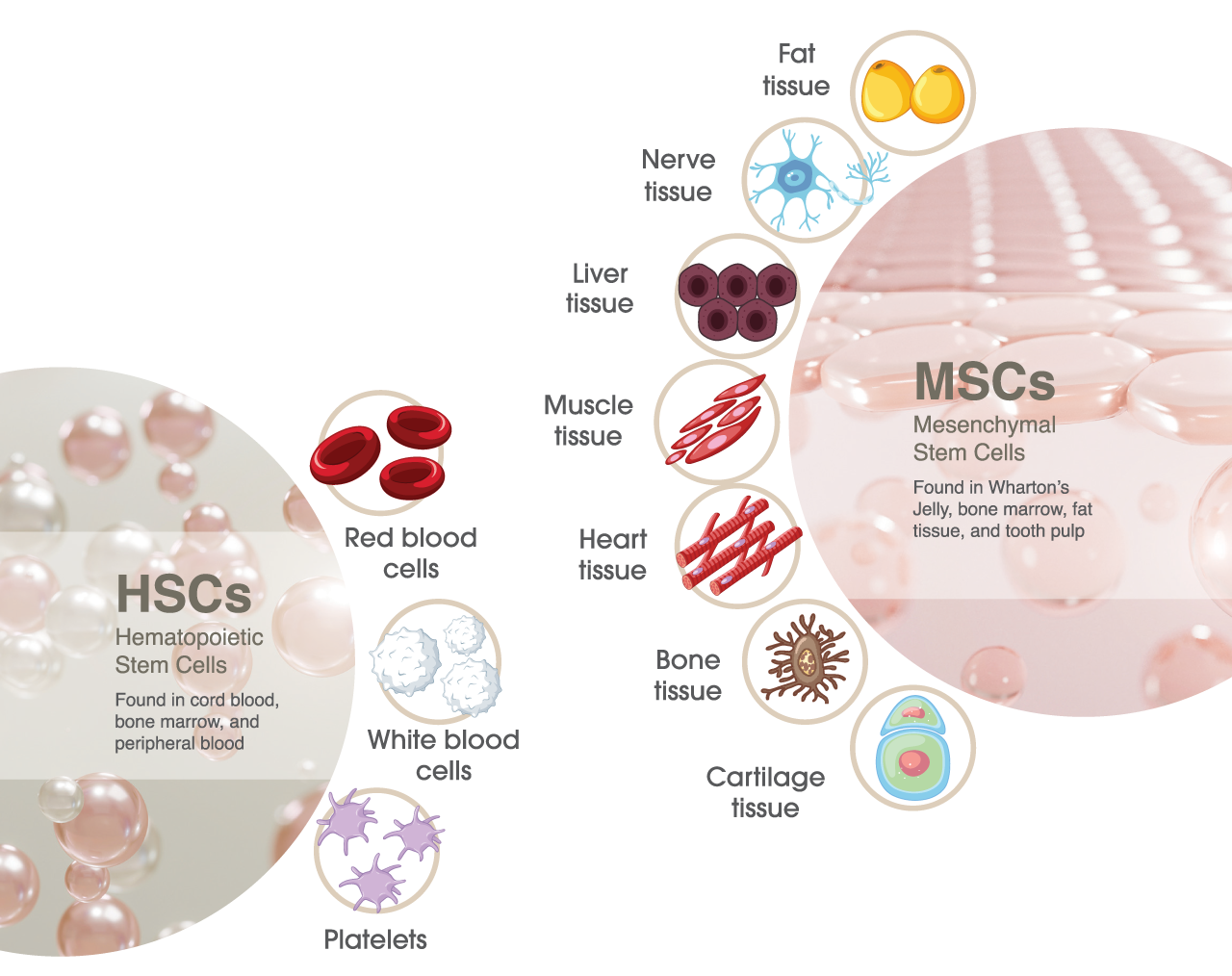
Mesenchymal Stem Cells are multipotent cells that can differentiate into a variety of cell such as fat cells, nerve cells, liver cells, muscle cells, heart cells, bone cells, and cartilage cells.
Electric Field Therapy – Improve Sleep and Reduce Risk of Dementia
Electric Field Therapy was shown to disrupt the process of amyloid aggregation, which is a substance that accumulates in the brain of those with Alzheimer’s disease, hence potentially slowing down disease progression. Electric field therapy has also been shown to improve sleep in those with sleep disorders, indirectly also mitigating those individuals’ risk for Alzheimer/dementia.
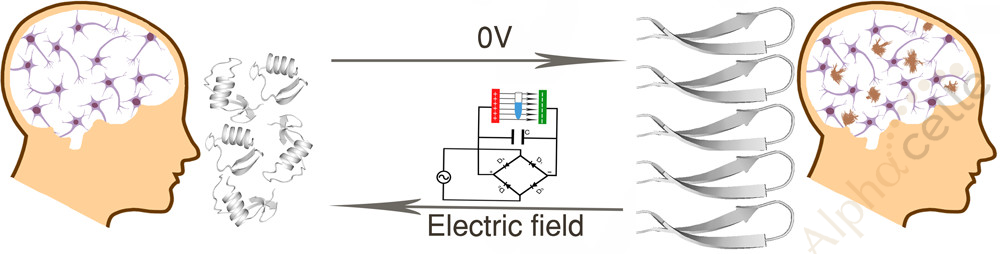
Source: ACS Publications
In conclusion, MSC and Electric Field Therapy combination might be a novel approach to prevention and potentially treatment of Alzheimer’s Disease or dementia.
